This has not been a good week for reporting on Military Medicine. Early this week U.S.News published a scathing article stating that the military’s ability to deliver outstanding care to wounded Soldiers is hindered by a lack of practice and continuing education. (https://www.usnews.com/…/surgeons-give-damaging-assessments…)
This was followed by the New York Time’s account of a tragic failure to manage the airway of a Soldier caught by a blast in Somalia. The medic failed to properly place, then failed to secure the surgical airway. Then the flight medics, upon noting poor BVM compliance, failed to reassess the intervention. The result was that SSG Alex Conrad suffocated to death. (https://www.nytimes.com/…/world/…/soldier-death-somalia.html)
Admittedly, the reporting is sensational as is common in this age. However, they ring of a hurtful truth. If these articles are accurate, this was a catastrophe for everyone involved. The lives of the patients, the families, the teammates of the casualties, and the medics are irreversibly altered. Eastridge et al. reported in 2011 that the rate of potentially survivable battlefield death for the conventional military was around 24%. What are we doing?
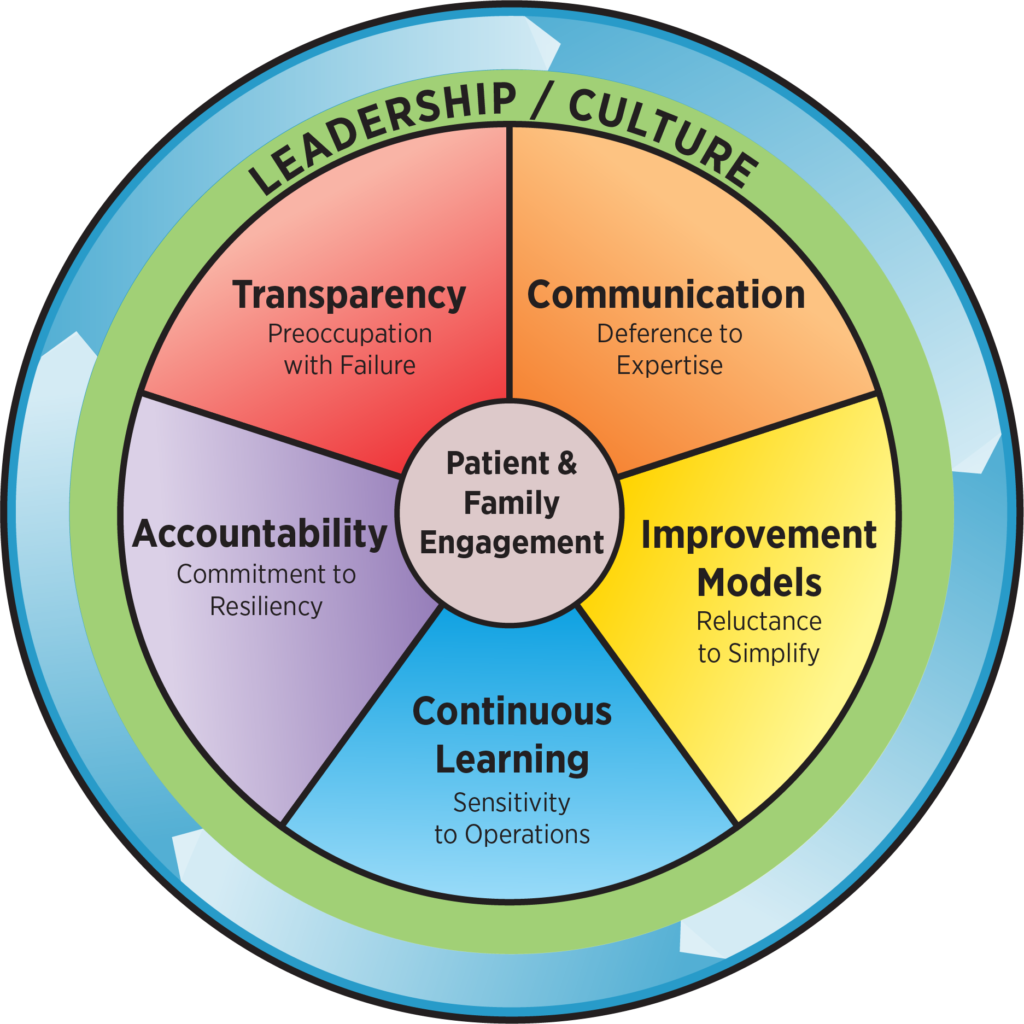
A key component of High-Reliability Organizations (HRO) involved in life and death operations is a “preoccupation with failure”. While this sounds very negative, it is an important part of identifying and fixing the causes of failure at an organizational level. If you aren’t familiar HROs, there is plentiful information available about the five principles. The Joint Commission has adopted the HRO model as a template for healthcare organizations across the nation.
Here is a sample plan of action for organizational remedial training for medical providers written by an experienced medical sergeant and educator over at Prolonged Field Care.
“I personally challenge you to complete the following action items this week. If we do not learn from our collective failure we will repeat it until we do.
There should be immediate notification, re-education, and retraining for everyone followed by an improved initial and sustainment training plan. Battalion Surgeons, PAs, Instructors, and Senior Medics should ensure every single medic does the following:
🛑 Receive the incident report and AAR from the Chain of Command the way other Saftey Stand Down incident reports are disseminated. Post it for the entire unit to read next to the parachute failure incident, ground accident report, or aircraft mishap report.
🛑 As a small group, read and review the report and AAR.
https://www.nytimes.com/…/world/…/soldier-death-somalia.html
🛑 Reread the guidelines and watch the videos freely available on the Deployed Medicine website or mobile app.
https://deployedmedicine.com/market/11/content/158
🛑 Ensure everyone immediately participates in hands-on tabletop training with whatever you currently have available or can easily construct.
https://emcrit.org/emcrit/ultimate-cricothyrotomy-trainer/
🛑 Discuss the shortfalls and inaccuracies of your trainer. Don’t just focus on the single skill, discuss other options that could have led to a better outcome:
❌ Could different patient positioning have helped the situation?
❌ How could the outcome have been different with various pharmacological adjuncts?
❌ Do you have supraglottic airways (SGA) in every aid bag? ❌ Do you have methods of verifying the placement of advanced airways? An Emma capnograph would have helped identify the false passage instantly. Even a colorimetric device may have helped.
❌ How well are non-Medics are trained to take care of an airway if it were the medic on the ground?
One of the things I have seen in small group training was to inject a hematoma just over the cricothyroid membrane. This makes it super messy and hard to identify landmarks which is usually a slam dunk training scar.
🛑 Submit a WRITTEN request through multiple channels for proper equipment. Cite the article, incident report, and TCCC guidelines as justification to your MEDLOG, S4, XO and anyone else who can affect the situation.
🛑 Identify training deficiencies in your immediate organization and actually make a WRITTEN request to your Command for additional remedial training to be included in future non-medical training. Attach the article to the request.
These are just a few things an HRO can EASILY and IMMEDIATELY accomplish. What else can you do to ensure this death of our brother is not in vain?”
I challenge everyone reading this post to take the situation into their own capable hands. Ensure the widest possible dissemination of the message. Ensure training is not only taking place but is preparing medics to perform on the battlefield. Lives continue to be at stake.


